Lower limb injuries
Lower limb injuries may involve hip bones, thigh, leg, and foot. It is a specialised part of the body for the support of weight, adaptation to gravity, and locomotion.
Hip Conditions
Groin pain
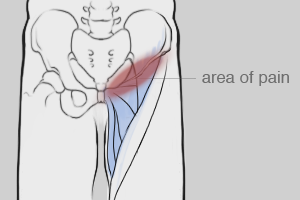
Groin strain involves a tear of the adductor muscle group (clearly defined large muscles on the inside of the thigh). The strain may occur with an overstretch or forceful contraction and therefore is frequently associated with sports, particularly those involving running and changing direction such as football and hockey
Muscle strain is classified in degrees, indicating severity (grade 1, 2 or 3). Early RICE management followed by graded gentle stretching and physiotherapy intervention can aid return to sport. Recurring groin strains often require a more in depth look at hip and leg biomechanics.
Other possible causes of groin pain can include injury to the abdominal muscles or their attachments (eg Gilmore’s Groin), pubic bone and hip bone stress injury or fracture (eg distance running). Pain in the groin may also be referred from areas such as the hip, pelvis and lower back.
Our physiotherapists will assess your symptoms and biomechanics, diagnose and ensure appropriate management of your pain.
Hip bursitis
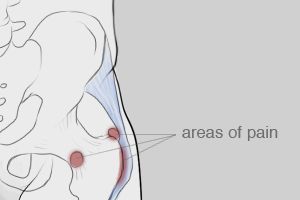
A bursa is a small fluid-filled sac that often sits between a tendon and bone preventing friction. Inflammation of the bursa (due to chronic irritation or acute trauma) is known as bursitis.
The bony point on the side of the hip is known as the greater trochanter – an attachment point for muscles. The trochanter has a bursa overlying it that can become irritated by certain activities or positions, causing pain on the side of the hip that is typically tender to touch (trochanteric bursitis).
Another bursa located on the inside of the hip near the groin is the deeper iliopsoas bursa. Iliopsoas bursitis usually causes pain around the groin.
Our physiotherapists can assess and provide treatment for bursitis. Treatment can target the local tissues to settle inflammation and address faulty postures, positions and muscle imbalances that may contribute to the problem. Injection may be helpful in more severe cases, and we can refer you to an appropriate specialist for this.
Piriformis syndrome
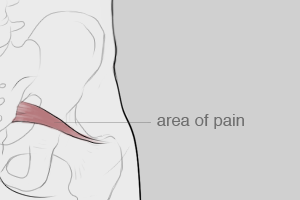
Piriformis is a muscle deep within the buttock. It may become painful if it becomes shortened or overactive over time, or it may go into spasm following injury. Pain can result from the compression or irritation of the sciatic nerve, which lies under or within the piriformis muscle.
Muscle shortening may be caused by prolonged poor postures or positions (eg sitting), or sitting combined with heavy leg muscle activity (eg cycling, rowing). Overactivity of the piriformis can arise in response to muscle imbalances – particularly weaker gluteal muscles, as these muscles are important for hip and pelvis stability. Seemingly unrelated biomechanical faults (eg pronation of the feet) may trigger piriformis syndrome due to the adaptive biomechanics. Our physiotherapists can assess and treat piriformis syndrome.
Treatment initially focuses on settling the pain, generally through manual therapy, electrotherapy, acupuncture, and often includes an exercise programme targeting weak and overactive muscles.
This is provided as general information only and is not intended to be relied upon as medical advice.
Knee Conditions
Ilio-Tibial Band Syndrome
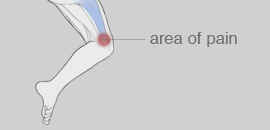
The iliotibial band (ITB) is a superficial tissue on the outside of the thigh, extending from the side of the pelvis and hip to just below knee. It helps stabilise the knee during running, and moves from behind the femur to the front while walking. The continual rubbing of the band over the lower end of the thigh bone, combined with the repeated movement of the knee during running may cause inflammation.
Sharp or stinging pain is most often felt in the outside of the knee, often caused by running. Classically, there is a biomechanical fault in the leg or foot which causes the band to become tight, and then rub at the knee. At times pain can be present on normal walking as the foot strikes the ground. Pain can extend up the thigh or lower down into the knee.
Treatment offered by our physiotherapy team can include manual therapy, off-loading and pain relieving techniques such as stretching and foam rolling, acupuncture, sports taping. Strengthening exercises can help reduce any muscle imbalance. Our physiotherapists can advise regarding orthotics, sporting technique and training.
Pes Anserine Bursitis

This is inflammation of a particular bursa on the inside of the leg just below the knee. A bursa is a sack of fluid that prevents friction between several tendons and the bone to which they attach.
Pes anserine bursitis commonly is characterized by pain, especially when climbing stairs and local swelling. It can be very tender to touch. It is most commonly caused by biomechanical faults in the leg and foot creating an overactivity or stress to the overlying tendon. Pain can also spread to knee joint.
We aim to treat this by settling the painful inflammation by manual therapy and other pain relieving techniques such as acupuncture, electrotherapy and taping. We will also assess your leg biomechanics which may need to be treated concurrently (often through exercise) to reduce contributing factors.
Fat pad impingement
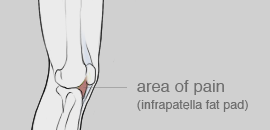
The fat pad below the patella (knee cap) is a soft tissue is at risk of being aggravated if the knee is hyperextended (over straightened).
When forces are directed at the patella it acts as a shock absorber, thus protecting the underlying structures. In the case of a forceful direct impact to the kneecap, the fat pad can become impinged between the femur (thigh) and the patella. As the fat pad is one of the most sensitive structures in the knee, this injury is extremely painful.
Symptoms include tenderness and/or swelling around the bottom of and under the kneecap. Symptoms are worse kneeling, squatting and climbing up and down stairs and/or hills.
We can assess and treat fat pad impingement by offloading the fat pad to settle pain and inflammation. Management may also include activity modification and addressing biomechanics through exercise. Our physiotherapists can both treat and guide you on your return to your chosen activities.
Patella Tendinopathy

An irritation, inflammation and/or tear to the patella tendon is known as a patella tendinopathy. This is the tendon attaching the quadriceps muscle on the front of the thigh to just below the knee. The symptoms are anterior knee pain, often with an aching quality during and particularly after activities. These symptoms are often gradual without history of trauma.
The condition is also referred to as Jumper’s knee, Patellar tendinosis or tendinitis. Occasionally it will progress to thickening of the tendon. It commonly occurs in athletes who are involved in jumping sports such as basketball and volleyball.
There are several causes of the problem, predominantly due to biomechanical faults throughout the leg or pelvis, ankle stiffness, gluteal muscle weakness, poor core stability, repetitive overactivity of the knee or leg length differences. Our physiotherapists will examine possible causes during assessment and direct treatment appropriately, as well as settling the local symptoms. We will guide you as you return to your sport or activity.
Popliteal muscle strain
The popliteus muscle is a thin, triangular muscle in the back of the knee. It bends the knee and rotates the leg. It is easy to strain or injure this muscle, especially if you are active and/or keen sports person as this muscle is an active stabiliser of the knee during physical activities while the leg is planted on the ground and the knee is rotating.
Once the popliteus is injured, the symptoms mainly involve pain and swelling at the back of the knee. The main aggravating factor, once the muscle has been injured, is prolonged sitting positions where the knee is bent and the popliteus muscle stiffens up in a shortened position. There are usually no symptoms of instability or locking of the knee but there is usually a history of trauma.
Download the knee information and exercise sheet
This is provided as general information only and is not intended to be relied upon as medical advice.
Ankle Conditions
Ankle Conditions
Ankle injuries are very common in sport but can also result from relatively trivial incidents such as turning the ankle when walking on uneven ground.
Lateral ligament sprain
The lateral ligaments lie on the outside of the ankle and can be injured by ‘going over’ on the ankle. This ligament is made up of 3 parts and the extent of the injury depends on the exact mechanism of the trauma. There is generally sharp pain, swelling and possible bruising with pain or difficulty weight-bearing.
In the early stages RICE (rest ice compression elevation) and protection of the ankle are most important. Our physiotherapists can assess the extent of your injury and use a range of techniques to settle the initial symptoms, then build on strength and coordination around the joint, supporting your return to sport.
Ankle impingement
Pain may occur at the back or front of the ankle that occurs with extreme movement or force. Anatomically two bones forming the joint pinch one another, more so if there is local bony enlargement due to repeated pressure or instability in the ankle. Our physiotherapists can help to establish the cause of your symptoms, help to settle the acute symptoms and can give advice regarding activity. Should your symptoms not respond to treatment we can refer you to a foot and ankle specialist for further management.
Achilles tendinopathy
This presents as pain and stiffness in the achilles, often with a difficulty walking when getting out of bed. Symptoms can occur gradually with overuse or suddenly as the result of a strain. in cases of severe strain or tear, a feeling of being hit in the achilles can occur, and may be accompanied by a bang.
Our physiotherapists can assess the extent of your achilles injury and identify the potential underlying causes. Treatment to settle initial symptoms will be followed by manual therapy, loading and strengthening, which will then be incorporated into a functional programme specific to your activity. In the event of diagnosing a complete tendon rupture, we will refer you to the orthopaedic specialist team for further management.
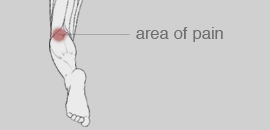
Ankle tendinopathy
The most commonly affected tendon is the tibialis posterior (muscle on the inside of the shin) and is associated with over pronation (foot flattening). This occurs in overloading or lack of support for the foot (e.g. increased running or running with worn out shoes). The tendon may show signs of inflammation, feeling slightly swollen or tender to touch on the inside of the ankle. Our physiotherapists will identify and manage the causes of your tendinopathy. Early treatment can include RICE, and further management may involve manual therapy to address stiff joints, and offloading the tendon through taping or use of orthotics can also help. We can refer on to a specialist podiatrist for custom made orthotics if required.
Shin splints
Shin splints can affect the muscle on the front or the inside of the shin. The muscle can pull on the bone, causing inflammation. This often occurs with poor training techniques or a sudden increase in training. Pain presents itself along the shin typically during or after exercise.
Our physiotherapists offer treatment to reduce the inflammation and pain. This will be followed by strengthening and weak or lengthened muscles, and addressing muscle imbalances that may contribute to the problem.
Inadequate rehabilitation of ankle injuries may result in persistent symptoms, reduced performance in sport and greater risk of recurrence.
Download the ankle information and exercise sheet
This is provided as general information only and is not intended to be relied upon as medical advice.